The Corrections Wellness Crisis: The Case for Investing in Officer Support Solutions
Posted
March 24, 2025
Share:
Introduction: A Growing Concern in Corrections
Over the past decade, a significant body of research has emerged that paints a concerning portrait of correctional officer wellness in the United States. While law enforcement personnel across various domains face challenging work environments, correctional officers face some of the most severe negative health outcomes in the entire public safety profession. Recent reviews describe correctional employees as “the unhealthiest of all law enforcement personnel,” with rates of post-traumatic stress disorder (PTSD) that approach or exceed those of military combat veterans (Health & Justice, 2024).
This alarming situation has led experts to warn that correctional staff are in the midst of a mental health “crisis,” marked by high prevalence of psychological disorders and even self-harm behaviors (Health & Justice, 2024). The implications extend beyond individual officers; chronic stress, burnout, and illness among correctional officers (COs) can undermine prison operations, safety, and staffing stability (National Institute of Justice, 2019).
This article examines the current state of correctional officer wellness, drawing on the latest research to highlight the need for modern, technology-enabled wellness solutions that can effectively address this crisis.
The Severity of the Problem: By the Numbers
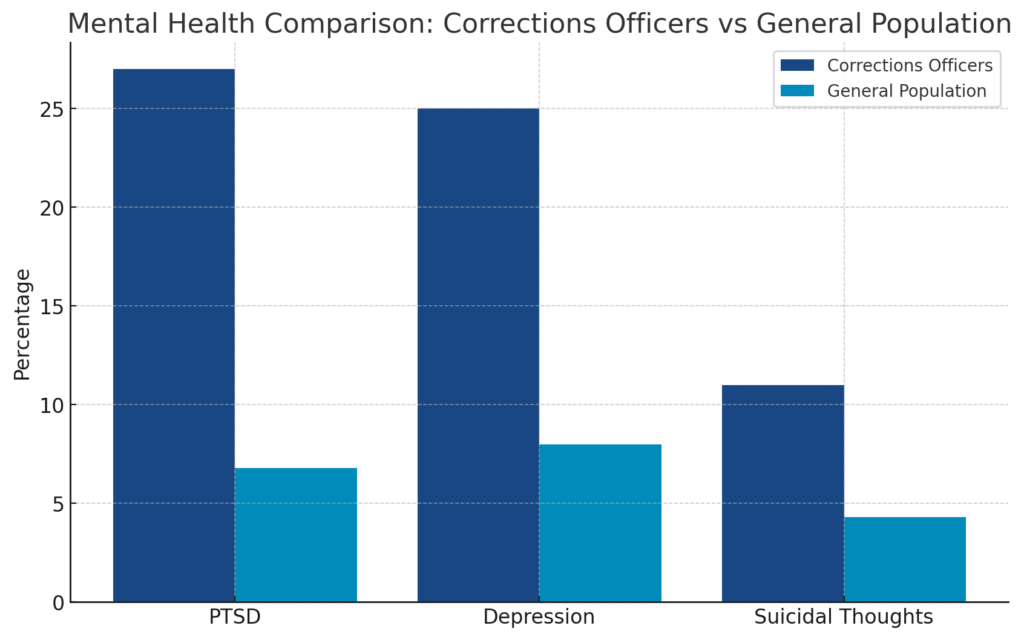
The statistics on correctional officer mental health are sobering:
- PTSD Prevalence: Between 19% and 34% of correctional officers suffer from PTSD, compared to approximately 6.8% in the general population (SIU, 2024). A national survey of nearly 3,600 correctional professionals found that 27% met the criteria for PTSD (Vera Institute, 2021). This is comparable to rates seen in veterans of the Iraq and Afghanistan wars and higher than those found among police officers (Prison Policy Initiative, 2022).
- Depression: Over 25% of correctional officers suffer from depression, with some state-level studies showing rates as high as 36% (Prison Policy Initiative, 2022). This is significantly higher than the general adult population rate of roughly 8% (National Institute of Mental Health, cited in SIU, 2024).
- Suicide Risk: correctional officers have a suicide rate 39% higher than the average for all other occupations (Vera Institute, 2021).
- Life Expectancy: The average life expectancy of a correctional officer is approximately 59 years—16 years shorter than the general U.S. population average of 75+ years (SIU, 2024).
- Mental Health Symptoms: In a 2021 survey of California prison staff, 48% reported feeling “anxious, nervous, or on edge” in the past month, 28% “felt down, depressed, or hopeless,” and 11% had experienced suicidal thoughts or attempts (Prison Policy Initiative, 2022).
These stark figures underscore the urgent need for effective interventions to protect the mental health and well-being of correctional officers.
Unique Stressors in the Corrections Environment
While many stressors faced by correctional officers resemble those in other law enforcement jobs, the correctional environment has unique characteristics that amplify the strain on staff:
1. Ever-Present Threat of Violence
COs must remain vigilant for inmate aggression, riots, assaults, and other dangers inherent to supervising often unwilling individuals. This leads to a state of chronic hypervigilance—always being on guard—which is mentally exhausting. One veteran American CO noted that while “95 percent” of the job might be mundane routine, the constant need to be alert for emergencies keeps officers in an elevated anxiety state (Vera Institute, 2021).
2. Unpredictable Hours and Overwork
Most correctional facilities are chronically understaffed, so officers frequently work mandatory overtime and double shifts. Schedules can be erratic, with rotating shifts, last-minute holdovers, and canceled days off (Vera Institute, 2021). Such conditions disrupt sleep patterns and family life, contributing to fatigue. Many COs report persistent exhaustion—80% in one survey felt tired even when coming on duty (Prison Policy Initiative, 2022).
3. Staffing Shortages and High Inmate Loads
Many prisons operate with fewer officers than needed. It’s common for a single CO to oversee large inmate dormitories or multiple units due to vacancies. These low officer-to-inmate ratios heighten risk and force officers to constantly triage their attention (The Carey Group, 2023). Understaffing also means less backup in dangerous situations and can leave officers feeling isolated and unsafe (National Institute of Justice, 2019).
4. Exposure to Trauma and Human Suffering
COs regularly witness traumatic events as part of the job—inmate suicides and self-harm, violent assaults, medical emergencies, and death (SIU, 2024). One national study found that 100% of COs had been exposed to at least one “violence, injury or death” incident in their career, with an average of 28 such events reported (OJP Research, cited in Health & Justice, 2024). Over years, this repeated exposure can lead to cumulative PTSD symptoms or desensitization.
5. Institutional Culture and Stigma
The corrections culture often includes a “macho” or stoic expectation to “be tough and ‘suck it up’” when facing hardship. Admitting to stress or seeking help has been stigmatized as a sign of weakness (Health & Justice, 2024). This culture of silence means problems fester until crisis points like breakdowns or disciplinary issues occur.
6. Lack of Public Recognition and Support
Unlike police or firefighters, correctional officers work behind the scenes with little public acknowledgment. Prison guards receive few public “thank yous” and may encounter negative perceptions. This relative invisibility can dampen morale and contribute to a sense of alienation.
7. Substance Abuse and Self-Medication
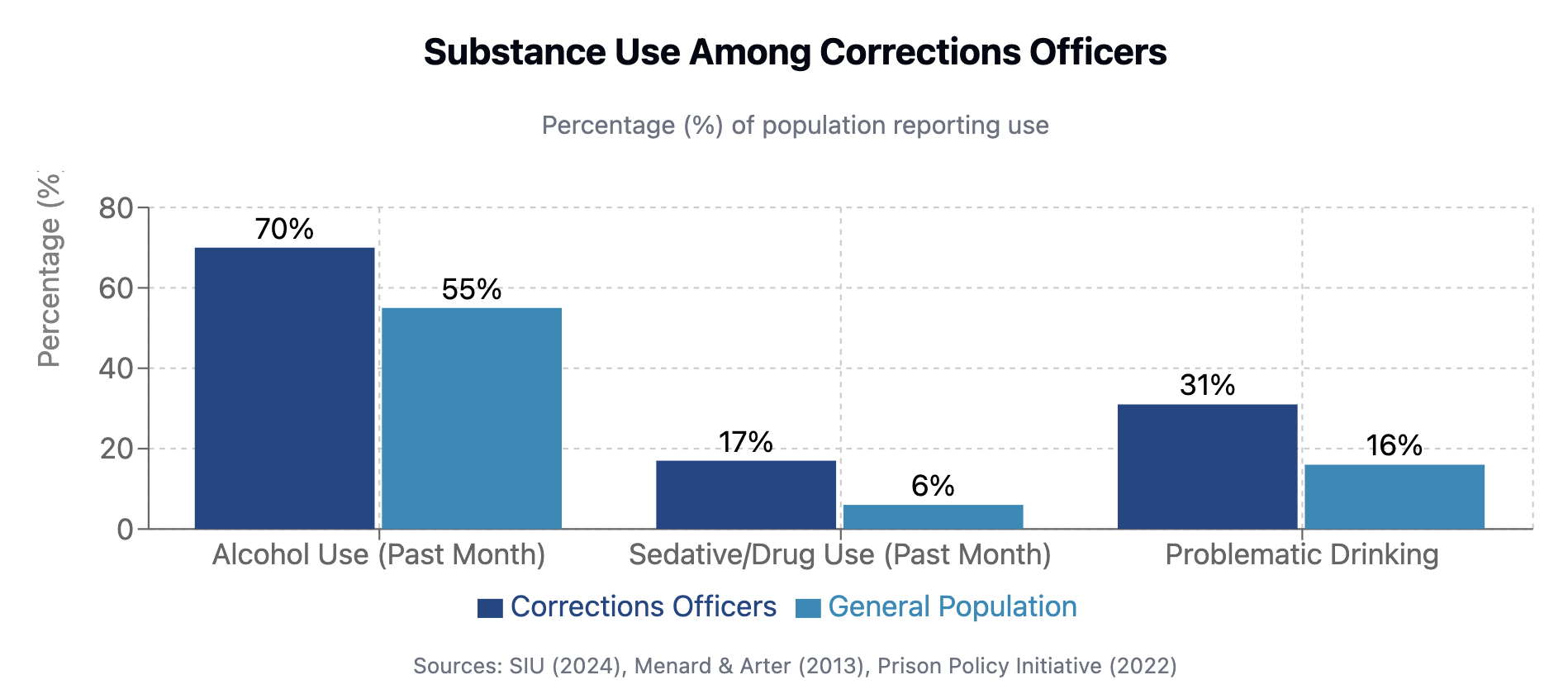 Many correctional officers turn to alcohol and other substances to cope with job-related stress, trauma, and sleep disruption. This problematic pattern of self-medication often worsens underlying mental health conditions while creating additional health risks.
Many correctional officers turn to alcohol and other substances to cope with job-related stress, trauma, and sleep disruption. This problematic pattern of self-medication often worsens underlying mental health conditions while creating additional health risks.
Research paints a concerning picture:
- In one study, over 70% of surveyed correctional officers reported using alcohol in the past month, and 17% reported using sedatives or other drugs, often as a coping mechanism for stress and sleep troubles (SIU, 2024).
- Officers who reported more exposure to critical incidents were more likely to engage in problematic drinking, with this relationship mediated by negative coping mechanisms (Menard & Arter, 2013).
- The rate of substance use disorders among correctional officers exceeds that of the general population by 30-40%, with many officers showing signs of dependence (Heyman et al., 2018).
- A 2021 California survey found that 31% of correctional officers reported “drinking more than intended” at least once in the previous month (Prison Policy Initiative, 2022).
The connection between trauma exposure and substance abuse creates a dangerous cycle. As Dr. Wasantha Jayawardene explains, “Many officers handle the stress by self-medicating with alcohol, prescription medications, or other substances, which can lead to dependency issues and worsen PTSD symptoms” (SIU, 2024).
This pattern of self-medication typically begins as an attempt to manage sleep problems, anxiety, or intrusive thoughts related to work experiences. However, it often develops into a dependency that further compromises officers’ health, judgment, and relationships (Menard & Arter, 2013).
Impact on Recruitment and Retention
The wellness crisis directly affects agencies’ ability to recruit and retain officers, creating significant operational challenges:

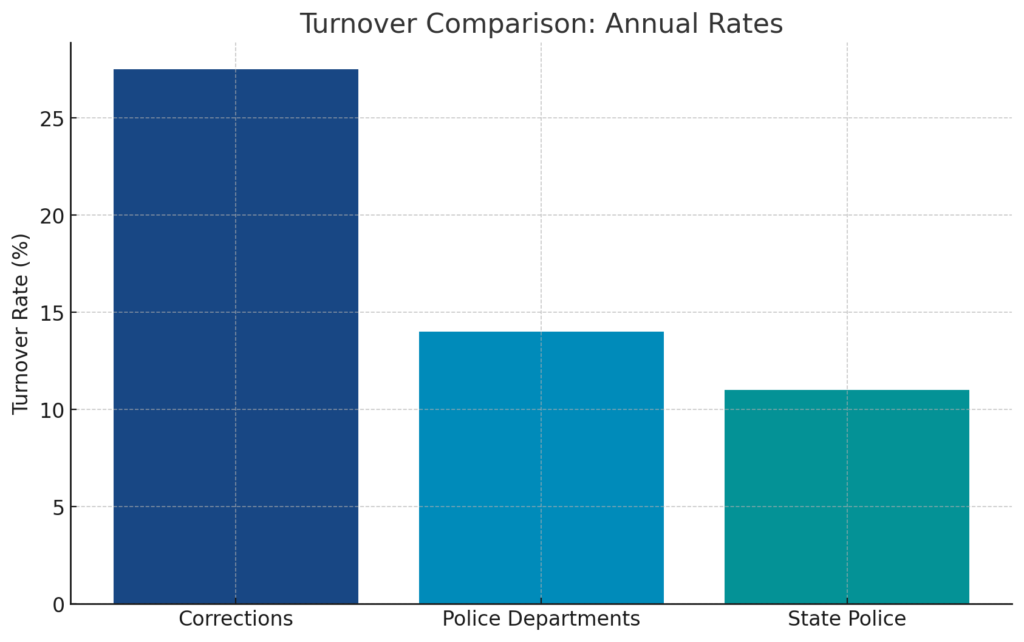
- High Turnover Rates: Nearly half of corrections agencies report annual officer turnover between 20% and 30% (Prison Policy Initiative, 2024), with some state systems exceeding 35% or even 100% in a single year (Alabama Department of Evidence Based Policing, 2024). By comparison, local police departments historically average around 10-15% turnover annually (All Star Talent, 2023).
- Early Departure: 38% of correctional staff leave within the first year and almost 50% leave within five years of employment (The Carey Group, 2023).
- Staffing Crisis: Between 2020 and 2023, the total number of people working in state and local corrections declined by about 12%, a loss of over 64,000 staff (Prison Policy Initiative, 2024).
- Operational Impacts: Understaffing forces facilities to limit normal operations, with frequent “lockdowns” due to lack of officers. Exhausted staff cover double shifts or posts they aren’t trained for, endangering inmates and further degrading working conditions (The Carey Group, 2023).
When officers quit in large numbers, the costs are immense—rising training and recruitment expenses, mandatory overtime demands, and safety risks from short staffing. According to the Bureau of Justice Statistics, by mid-2022 the ratio of incarcerated persons to correctional officers had risen to 4-to-1 (up from 3-to-1 in 2020) (The Carey Group, 2023).
The Current State of Wellness Programs
Despite growing awareness of these issues, the response from correctional institutions has often been inadequate:
Limitations of Current Approaches
- Reliance on Self-Reporting: Most wellness initiatives depend on officers voluntarily seeking help—an approach that fails to reach many in need due to stigma and the corrections culture (Health & Justice, 2024).
- Reactive Rather Than Proactive: Many departments only address wellness issues after a crisis occurs, rather than identifying at-risk officers early.
- Limited Evidence Base: Few correctional wellness programs are based on rigorous research or have been scientifically evaluated for effectiveness (National Institute of Justice, 2019).
- Inconsistent Implementation: Programs often lack structured follow-through and consistent application across facilities (The Carey Group, 2023).
- Inadequate Resources: Many agencies, particularly smaller ones, lack dedicated funding or staff for wellness initiatives (Prison Policy Initiative, 2022).
Mixed Evidence of Effectiveness
 Research on existing corrections wellness programs shows mixed results:
Research on existing corrections wellness programs shows mixed results:
- A 2017 Justice Department literature review noted that “few of these programs have been subjected to rigorous scientific evaluation, thus limiting the understanding of their effectiveness” (National Institute of Justice, 2019).
- One study of an enhanced Employee Assistance Program (EAP) for corrections staff showed some initial improvements in resilience, but these effects “vanished” after more stringent statistical tests (Research Gate, 2010).
- A 2025 academic assessment concluded: “Research has evaluated the ability of [wellness] programs to improve correctional officer wellbeing. Overwhelmingly, either studies found no improvements, or in the rare cases where they did, their methodological designs were flawed” (Research Gate, 2010).
These findings suggest that current approaches are insufficient to address the scale of the wellness crisis in corrections.
The Need for Comprehensive, Technology-enabled Solutions
To effectively address the unique challenges of correctional officer wellness, agencies need more sophisticated, research-based approaches:
1. Data-Driven Identification of At-Risk Officers
Rather than relying solely on self-reporting, modern wellness solutions should leverage existing data to identify officers who may be struggling proactively. This includes:
- Analyzing exposure to traumatic incidents and tracking cumulative impact
- Monitoring work patterns that indicate fatigue or exhaustion
- Identifying anniversary dates of significant incidents that may trigger stress responses
- Tracking indicators of burnout or distress in workplace behaviors
This approach allows agencies to intervene before a crisis occurs, potentially saving careers and lives.
2. Structured Support and Case Management
When an officer is identified as potentially at risk, agencies need structured systems to:
- Guide supervisors through wellness conversations using evidence-based scripts and checklists
- Create and document personalized wellness plans
- Ensure consistent follow-up and assessment of progress
- Connect officers to appropriate resources based on their specific needs
These systems help overcome supervisors’ discomfort when addressing wellness issues and ensure that officers receive consistent support.
3. Research-Proven Interventions
Any effective wellness solution must include interventions with demonstrated efficacy:
- One randomized controlled trial of wellness interventions for police officers showed significant benefits, including:
- 18 additional minutes of sleep per night
- 2-point reduction in self-reported depression scores
- 50% reduction in self-reported PTSD symptoms
- 33% reduction in self-reported anxiety symptoms
- 45% reduction in episodes of falling asleep while driving
(Seattle Trauma Study, 2024; Benchmark Analytics Wellness Research, 2024)
Such evidence-based content should focus on building resilience before crises occur, not just managing them afterward.
4. Comprehensive Clinical Support
While technology can facilitate wellness initiatives, human support remains crucial:
- 24/7 access to crisis resources for officers in immediate need
- Culturally competent clinicians who understand the unique stressors of corrections work
- A bridge to connect officers with longer-term mental health services when needed
- Support for supervisors who are helping officers through wellness challenges
This clinical component ensures that officers receive expert guidance when facing serious mental health issues.
The Return on Investment: Why Wellness Solutions Make Financial Sense
Beyond the human benefits, investing in correctional officer wellness delivers measurable financial returns:
1. Reduced Turnover Costs
The cost of replacing an officer includes recruitment, academy training, field training, and lost productivity while positions remain vacant. Reducing turnover by even a small percentage can result in significant savings (The Carey Group, 2023).
2. Decreased Overtime Expenses
When staffing levels stabilize, the need for expensive mandatory overtime decreases, providing immediate budget relief (Prison Policy Initiative, 2024).
3. Lower Workers’ Compensation and Disability Claims
Officers with better mental health are less likely to develop stress-related physical conditions that lead to time off and claims (Mumford et al., 2021).
4. Improved Facility Safety and Reduced Incidents
Well-rested, mentally healthy officers make better decisions, potentially reducing costly incidents and litigation (National Institute of Justice, 2019).
5. Enhanced Recruitment Potential
Agencies that support officer wellness gain advantages in recruiting new personnel in a competitive market (Alabama Department of Evidence Based Policing, 2024).
One state agency analysis found that the cost of replacing correctional officers due to turnover exceeded $16 million annually (Alabama Department of Evidence Based Policing, 2024). Investing a fraction of this amount in wellness technology could significantly reduce these expenses.
Conclusion: The Path Forward
The wellness crisis in corrections isn’t just a personnel issue—it’s a strategic challenge that affects facility operations, public safety, and fiscal responsibility. The research clearly demonstrates both the severity of the problem and the inadequacy of current approaches (Health & Justice, 2024).
Modern, technology-enabled wellness solutions offer a promising path forward by combining:
- Proactive identification of officers at risk
- Structured guidance for wellness conversations and planning
- Evidence-based interventions proven to improve well-being
- Comprehensive clinical support for officers in need
As the corrections field continues to face staffing challenges and operational pressures, investing in officer wellness isn’t just the right thing to do—it’s a strategic necessity for agencies seeking sustainable operations and fiscal responsibility (Mumford et al., 2021).
The question for correctional leaders isn’t whether they can afford to invest in officer wellness—it’s whether they can afford not to.
For more information on evidence-based wellness solutions for correctional officers, contact us to learn how modern wellness platforms are transforming officer support in corrections agencies nationwide.
References
Correctional officers and the ongoing health implications of prison work. Health & Justice. (2024).
National Institute of Justice. (2019). Correctional Officer Safety and Wellness: What We Learned from the Research Literature.
Prison Policy Initiative. (2022). Working in “a meat grinder”: A research roundup showing prison and jail jobs aren’t all that states promise they will be.
Prison Policy Initiative. (2024). Why jails and prisons can’t recruit their way out of the understaffing crisis.
Vera Institute. (2021). Reimagining Prison: The Prison Experience for Corrections Staff.
SIU researchers find prison guards suffer PTSD and other issues but get little help. (2024).
Alabama Department of Evidence Based Policing. (2024). Correctional Officer Recruitment and Retention Efforts.
The Carey Group. (2023). Reducing Corrections Staff Turnover Through Evidence-based Strategies.
Heyman, M., Dill, J., & Douglas, R. (2018). Mental health and suicide of first responders: Recommendations for action. Ruderman Family Foundation.
Lawrence, D. S., Padilla, K. E. L., & Dockstader, J. (2025). Bearing the badge, battling inner struggles: Understanding suicidal ideation in law enforcement. Journal of Police and Criminal Psychology.
Seattle Trauma Study. (2024). Evaluating the effectiveness of a fatigue training intervention for the Seattle Police Department: Results from a randomized control trial.
Mumford, E. A., Taylor, B. G., Liu, W., Barnum, J., & Goodison, S. (2021). Law enforcement officers’ safety and wellness: A multi-level study. National Institute of Justice.
Taylor, B. G., Liu, W., & Mumford, E. A. (2021). A national study on the availability of law enforcement agency wellness programming for officers: A latent class analysis. International Journal of Police Science & Management.
Menard, K. S., & Arter, M. L. (2013). Police officer alcohol use and trauma symptoms: Associations with critical incidents, coping, and social stressors. International Journal of Stress Management, 20(1), 37-56.
Related Posts
Ready to Experience the Benchmark Difference?
Benchmark Analytics and its powerful suite of solutions can help you turn your agency’s challenges into opportunities. Get in touch with our expert team today.



